How to Implement HIPAA Training for Providers

Key Takeaways
How to Implement HIPAA Training for Providers
HIPAA training is mandatory for everyone handling patient data. Here's how to ensure compliance while protecting sensitive information:
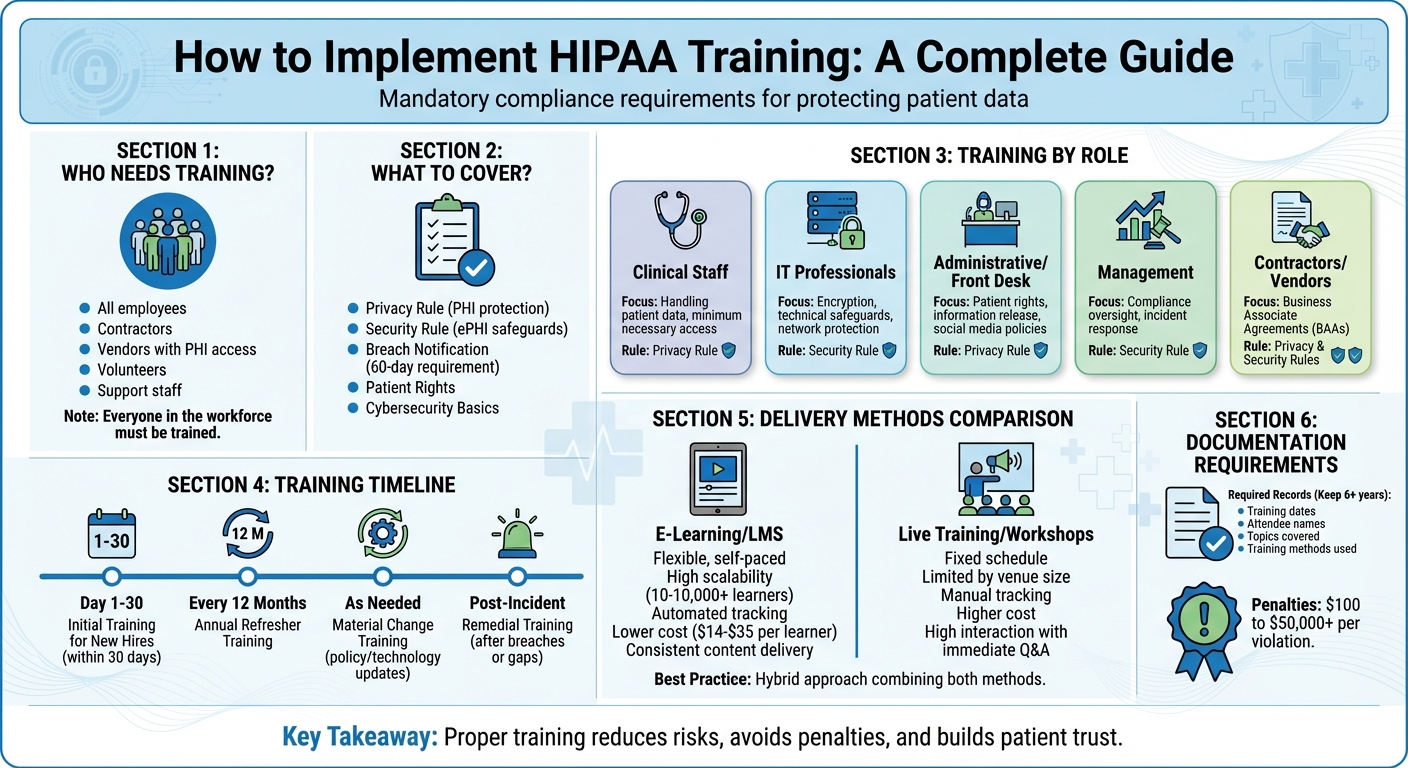
- Who Needs Training? Everyone in your organization, including employees, contractors, and vendors with access to Protected Health Information (PHI).
- What to Cover? Privacy and Security Rules, breach notification, patient rights, and cybersecurity basics.
- How to Train? Use e-learning platforms for flexibility or live workshops for interaction. A hybrid approach often works best.
- When to Train? New hires need training within 30 days. Offer annual refreshers and additional sessions for updates or breaches.
- Tracking Progress: Document all training activities, including dates, attendee names, and topics, for at least six years.
Proper training reduces risks, avoids penalties, and builds trust with patients. Tailor content to roles, use real-world scenarios, and ensure everyone understands their responsibilities.
HIPAA Training Implementation Timeline and Requirements
HIPAA Staff Training Updated for 2024 (MAJOR CHANGES)
sbb-itb-8f61039
Assessing Training Needs and Requirements
Figuring out who needs HIPAA training and what they should learn is a critical first step. HIPAA regulations are designed to be flexible, so there’s no universal training program. The Office for Civil Rights (OCR) clarifies this flexibility:
"The HIPAA Rules are flexible and scalable to accommodate the enormous range in types and sizes of entities that must comply with them. This means that there is no single standardized program that could appropriately train employees of all entities."
This adaptability allows organizations to tailor their training based on their size, structure, and workflows. The next step? Identifying exactly who needs to be trained.
Identifying Who Needs Training
Every member of the workforce must complete HIPAA training. This includes more than just doctors and nurses. Employees, volunteers, contractors, and even support staff who might come into contact with Protected Health Information (PHI) are part of this requirement . According to the Security Rule (CFR 45 § 164.380), both Covered Entities and Business Associates must provide security awareness training to all workforce members, including management, regardless of their level of PHI access.
Start by creating a detailed list of everyone in your organization, including third-party vendors who handle PHI. If a vendor processes data on your behalf, they also need training, particularly around Business Associate Agreements (BAAs) and their obligations. To ensure inclusivity, provide training in the primary languages spoken by your workforce.
Once the audience is identified, customize training objectives to fit the specific responsibilities of each role.
Setting Training Goals by Role
After determining who needs training, tailor the content to match each role’s job functions and level of PHI access. The Privacy Rule specifies that training should be "as necessary and appropriate for members of the workforce to carry out their functions" . For instance, clinical staff who regularly handle patient records require different training than someone who might only pass through areas where PHI is visible.
Using a modular approach can help avoid information overload. For example:
- IT professionals need in-depth training on encryption, access controls, and securing networks.
- Front desk staff should focus on patient rights, the Notice of Privacy Practices, and avoiding privacy breaches during phone calls or on social media.
- Management needs to understand security awareness and how to foster a compliance-driven culture.
Training should align with the "minimum necessary" standard, ensuring employees only access PHI essential to their roles. As Monica McCormack from Compliancy Group explains:
"Healthcare workers that access patient records outside of their job function are violating HIPAA. This is why healthcare workers should only have access to the PHI that they need for their job"
Every employee should understand what PHI they can access and why those boundaries are in place.
| Role Group | Primary Training Focus | Key HIPAA Rule |
|---|---|---|
| Clinical Staff | Handling patient data, PHI disclosure, "minimum necessary" access | Privacy Rule |
| IT Professionals | Encryption, technical safeguards, ePHI security, network protection | Security Rule |
| Administrative/Front Desk | Patient rights, release of information, social media policies | Privacy Rule |
| Management | Compliance oversight, incident response, security awareness | Security Rule |
| Contractors/Vendors | Business Associate Agreements (BAAs), shared responsibilities | Privacy & Security Rules |
Collaborate with HR, IT managers, and practice managers to identify any upcoming changes - like new roles, hardware, or software - that might require specialized training modules. Regular risk analyses can also help uncover knowledge gaps that need addressing. This teamwork ensures your training program stays relevant and supports everyday operations effectively.
Creating Training Modules
After identifying who needs training and understanding the specific requirements for each role, the next step is creating effective training content. Your modules should thoroughly address HIPAA compliance standards while staying relevant to your team’s daily tasks. The key is to strike a balance between being comprehensive and practical - no one benefits from long-winded, jargon-heavy lectures.
Instead of cramming everything into one extended session, divide your training into shorter, focused modules. According to CalHIPAA, "when training goes on for too long, only a limited amount of information is retained. Therefore, it is better to schedule a specific number of modules per session for advanced training programs". For basic sessions, aim for 1–2 hours, while advanced topics may require multiple sessions. This modular approach prevents information overload and gives staff the chance to process and retain what they’ve learned.
To make the training more engaging, incorporate interactive elements such as quizzes, case studies, and security simulations. Hook Security emphasizes that "providing dry, boring training can lead to low engagement and low retention of information. Using interactive and engaging training materials can help increase employee engagement".
Required Topics to Cover
Every HIPAA training program must include several essential topics:
- Privacy Rule: Explain Protected Health Information (PHI), the "minimum necessary" standard, and the permitted uses and disclosures for Treatment, Payment, and Healthcare Operations (TPO).
- Patient Rights: Cover rights like accessing medical records, requesting amendments, obtaining an accounting of disclosures, and receiving a Notice of Privacy Practices (NPP).
- Security Rule: Focus on protecting electronic PHI (ePHI) through the "CIA" triad - Confidentiality, Integrity, and Availability. Address administrative, physical, and technical safeguards, such as encryption and access controls. IT staff may need more detailed training, while others require enough knowledge to follow established protocols.
- Breach Notification: Define breaches, the 60-day notification requirement, and reporting procedures. Highlight that breaches affecting fewer than 500 individuals must be reported annually, while larger incidents require immediate notification.
- Modern Cybersecurity: Teach phishing recognition, password management, and the risks of unsecured Wi-Fi or mobile devices. Include guidelines for professional communication and enforce social media policies that prohibit sharing identifiable patient information.
- Consequences of Non-Compliance: Discuss the legal, financial, and reputational risks for both the organization and employees.
| Rule | Primary Focus | Core Training Topics |
|---|---|---|
| Privacy Rule | Patient Rights & PHI Use | PHI definitions, TPO disclosures, rights to access/amend, Notice of Privacy Practices (NPP) |
| Security Rule | ePHI Protection | Administrative, physical, and technical safeguards; encryption; password management; CIA triad |
| Breach Notification | Incident Response | Breach definitions, risk assessment, 60-day notification timeline |
Don’t forget to address any additional state-specific privacy laws that go beyond federal HIPAA requirements. Including these ensures your training is fully compliant.
Using Real-World Examples
Real-world examples make HIPAA training relatable and easier to understand. Create drills based on common scenarios, such as a nurse managing a phone inquiry from someone claiming to be a patient’s family member or an IT technician handling a suspicious email from a vendor.
Avoid simply reading HIPAA rules aloud. CalHIPAA warns that "the terminology is often difficult to follow audibly". Instead, translate the rules into practical examples. For instance, show front desk staff how to verify a caller’s identity before sharing information or teach clinical staff how to maintain patient privacy in public areas.
Highlight examples of incidental disclosures to clarify what doesn’t qualify as a violation. When employees see the real-world consequences of actions like leaving an unencrypted laptop unattended, they’re more likely to take compliance seriously.
Tailor these scenarios to specific roles within your organization, and document all training efforts. HIPAA requires you to keep records of topics covered, training dates, attendee names, and methods used for at least six years. These practical, role-specific examples reinforce the importance of compliance, ensuring your training is both effective and memorable.
Choosing Training Delivery Methods
Once you've developed targeted HIPAA training modules, the next big decision is how to deliver them in a way that keeps your team compliant and engaged. The HIPAA Rules allow for flexibility in delivery methods, so there's no one-size-fits-all approach. The best choice depends on factors like your team's size, budget, and whether your workforce is centralized or spread out. This step is key to ensuring that your training approach aligns with your organization's unique needs.
The two primary options are e-learning platforms (such as Learning Management Systems) and live training sessions. Many organizations find a hybrid approach works best - using online modules for foundational knowledge and in-person workshops to address specific policies and more nuanced questions. This mix combines the efficiency of digital training with the personalized interaction of face-to-face sessions.
When deciding, make sure to prioritize tracking and documentation, as HIPAA requires training records to be kept for at least six years. E-learning platforms often simplify this with automated reports and instant certifications. On the other hand, tracking attendance for live sessions requires more manual effort, which could lead to errors during audits.
Flexibility is also important. Healthcare workers, for example, may struggle to attend scheduled sessions due to shift work and patient care. Platforms that save progress and work seamlessly on mobile devices allow staff to complete training during breaks or from home. According to CalHIPAA:
"online HIPAA training can be just as effective as in-person training, especially when designed interactively with assessments, real-life scenarios, and multimedia content".
E-Learning and Learning Management Systems (LMS)
E-learning platforms are ideal for scalability. Whether you’re training a small team or thousands of employees, these tools eliminate the need for scheduling conflicts or physical space. Modern LMS platforms offer 24/7 access on any device, automated tracking with compliance reports, and regular content updates to reflect regulatory changes. This ensures consistent training across your entire organization.
Pricing for online HIPAA training typically starts at $14.00 per person, with bundled packages averaging $35.00 per learner. Many providers offer volume discounts for organizations training 10 or more employees. If your organization is growing, consider "pay-as-you-go" models with per-seat pricing. These allow you to scale costs as your team expands without committing to large upfront investments.
When evaluating LMS options, prioritize security features. The platform itself must be HIPAA-compliant, with robust encryption, multi-factor authentication (MFA), and strict access controls. Integration with existing HR systems is also critical to avoid data discrepancies and reduce manual work.
One common challenge with e-learning is user resistance. Some employees may view online training as a box-ticking exercise. To counter this, involve staff in selecting the platform and choose one with engaging features like quizzes, case studies, and multimedia content. Gamification elements - like leaderboards, rewards, and scenario-based challenges - can also boost participation and foster a sense of healthy competition.
Live Training and Workshops
While e-learning offers efficiency and scalability, live training excels in real-time interaction. These sessions are particularly effective for addressing complex topics, facilitating Q&A, and tailoring discussions to your organization's specific policies and procedures. This format allows employees to gain clarity on nuanced issues that generic training materials might overlook.
Live training also emphasizes the importance of compliance. When senior management participates alongside staff, it reinforces the message that HIPAA compliance is a priority. Additionally, these sessions help build rapport between employees and compliance officers, making staff more comfortable seeking guidance later.
However, live training comes with logistical challenges. Costs can add up quickly, considering venue rentals, travel expenses, and lost productivity, especially for organizations with multiple locations. Additionally, attendance and completion must be tracked manually, which increases administrative workload compared to automated LMS systems.
A hybrid model often strikes the right balance. Use e-learning for universal HIPAA concepts and supplement with shorter live sessions for role-specific scenarios, recent incidents, or policy updates. This approach combines the efficiency of digital tools with the engagement of in-person interactions.
| Feature | E-Learning / LMS | Live Training / Workshops |
|---|---|---|
| Scheduling | Flexible; self-paced | Fixed; requires coordinating schedules |
| Scalability | High; train 10 to 10,000+ learners | Limited by venue size and trainer availability |
| Tracking | Automated progress and certifications | Manual attendance tracking |
| Cost | Lower per learner with volume discounts | Higher costs due to trainers and logistics |
| Interaction | Interactive via quizzes and multimedia | High; immediate Q&A and discussions |
| Consistency | Uniform content delivery | Variable; depends on trainer and session |
Setting Up Training Schedules and Tracking Progress
Once you've chosen your training delivery methods, the next step is to create a structured schedule and tracking system to meet HIPAA compliance requirements. HIPAA mandates that all training activities be documented. Failing to properly schedule and track these activities can lead to compliance gaps, which carry penalties ranging from $100 to $50,000 or more per violation.
It's important to strike a balance between meeting regulatory requirements and creating a practical schedule. This includes planning initial training for new hires, annual refresher sessions for current staff, and additional training when policies or technologies are updated.
Planning Training Timelines
New hires should complete their training within 30 days of starting. HIPAA regulations require training within a "reasonable period" after someone joins your organization, and most healthcare providers aim for the first 30 days to ensure employees understand their responsibilities before handling protected health information (PHI).
To make training manageable, consider modular sessions tailored to specific roles. Instead of a lengthy five- to six-hour session, break the content into smaller, focused blocks. For instance:
- Front-desk staff could complete a 30-minute module on patient check-in procedures.
- IT personnel might focus on a separate module covering technical safeguards.
This approach minimizes disruptions to patient care and helps prevent information overload.
Offering Continuing Education Units (CEUs) can further motivate employees to complete their training on time.
| Training Type | Trigger/Frequency | Target Audience |
|---|---|---|
| Initial Training | Upon hire (within a "reasonable period") | All new employees, volunteers, and interns |
| Annual Refresher | Every 12 months | All existing workforce members |
| Material Change | Policy, procedure, or technology updates | Impacted workforce members |
| Remedial Training | Following a breach or risk assessment gap | Involved staff or specific departments |
Once your timelines are established, document all training completions to ensure compliance with these schedules.
Recording Training Completion
To meet the requirements of 45 CFR § 164.530, you need to document essential details like attendee names, training dates, topics covered, and methods used. This documentation not only supports compliance audits but also helps identify any training gaps.
One effective method is to have employees sign acknowledgment forms - either physical or digital - confirming they have received and understood the training materials. Steve Alder, Editor-in-Chief of HIPAA Journal, highlights:
"Trainees should sign attestations to confirm they have received training if progress is not monitored by a learning management system".
For live sessions, attendance can be tracked manually using spreadsheets or HR software.
Collaboration between HR and IT departments is crucial for seamless tracking. HR can flag new hires for immediate training enrollment, while IT can issue retraining alerts when systems or software are updated. As noted by CalHIPAA:
"Don't forget to maintain a record of training sessions and attendees. This is necessary should a breach occur, as it shows that the organization was following HIPAA training requirements".
Keep these records for at least six years.
With training completions properly documented, the next step is to evaluate the program's effectiveness through targeted assessments.
Measuring Training Results
To determine whether your training is effective, use tools like post-training quizzes, scenario-based drills, and compliance monitoring. Quizzes, administered during or immediately after training, provide a quick snapshot of how well employees have retained the material.
Scenario drills are another way to test real-world application of HIPAA rules. For instance, you could present a situation where an employee receives a phone call requesting patient information. Their response can reveal whether they've fully understood the training.
Monitoring compliance metrics, such as data breaches or policy violations, offers additional insights. A decrease in incidents after training is a strong indicator of success. However, if issues persist in specific departments, it may signal the need for more targeted retraining.
Employee feedback is invaluable for refining your program. Surveys can highlight areas where the training felt unclear, too lengthy, or irrelevant to certain roles. Internal audits also help identify knowledge gaps and confirm that all necessary personnel have been trained.
Conclusion
To wrap things up, let’s revisit the key steps for creating a solid HIPAA training program that balances compliance with practical, day-to-day application.
Start by identifying all staff members who need training and tailor the content to fit their specific roles. As the Office for Civil Rights highlights:
"The HIPAA Rules are flexible and scalable to accommodate the enormous range in types and sizes of entities that must comply with them. This means that there is no single standardized program that could appropriately train employees of all entities."
Focus on the core HIPAA rules, using relatable, real-world examples to make the material more engaging and easier to apply. Choose the best delivery method for your organization - whether that’s through e-learning platforms, live workshops, or a mix of both. Set clear timelines for onboarding new hires and ensure annual refreshers are part of your schedule.
Regularly assess your program with tools like quizzes, scenario-based exercises, and compliance tracking. These help you catch and address knowledge gaps before they turn into costly violations. Non-compliance can result in hefty penalties, so thorough documentation and ongoing evaluation are essential for safeguarding both your organization and your patients.
Lastly, involve leadership in the training process. When leaders participate alongside staff, it underscores the importance of data security and creates a company-wide culture of compliance. This not only strengthens internal practices but also builds trust with patients, showing them that protecting their health information is a top priority. By refining your training program based on feedback and outcomes, you can ensure it remains effective and keeps your organization compliant while safeguarding sensitive patient data.
FAQs
What’s the difference between e-learning and live training for HIPAA compliance?
E-learning and live training take different approaches to HIPAA compliance education, each with its own strengths.
E-learning stands out for its flexibility. It’s self-paced, allowing healthcare providers to fit training into their own schedules. With features like videos, quizzes, and simulations, it keeps learners engaged while making progress easy to monitor. Plus, it’s adaptable - specific modules can be tailored to staff roles, ensuring relevant training for everyone.
Live training, in contrast, involves an instructor leading sessions, either in person or through webinars. This format encourages real-time discussions and provides immediate answers to questions, which can be particularly helpful for tackling complex topics. However, it does require participants to commit to a set time and place, which might be challenging for busy professionals.
Each method has its perks. E-learning shines in convenience and customization, while live training offers a more interactive and hands-on experience. The right choice will depend on your organization’s priorities and scheduling needs.
How can healthcare organizations ensure their employees understand their HIPAA responsibilities?
Healthcare organizations must ensure their employees fully grasp their HIPAA responsibilities by implementing a targeted, role-specific training program paired with consistent reinforcement. Start by identifying everyone who needs training - this includes full-time and part-time employees, contractors, and volunteers. Then, customize the training to match their roles. For instance, clinicians should focus on properly handling PHI (Protected Health Information), while IT staff should prioritize password protocols and data security measures.
Keep the training straightforward and easy to digest by using modular content. This helps prevent information overload and ensures the material stays relevant. Training sessions can be conducted online or in person, with completion verified through signed acknowledgments or quick quizzes. To keep HIPAA principles top of mind, reinforce them regularly through tools like newsletters, short videos, or phishing simulations. Additionally, use training reports to track compliance and address any gaps as soon as they arise.
By following these practices, healthcare organizations can build a strong culture of compliance, ensuring every team member is prepared to uphold HIPAA standards effectively.
What should you do if a HIPAA breach occurs despite training?
If protected health information (PHI) is compromised despite HIPAA training, taking immediate action is critical to reduce potential harm. Begin by implementing your organization’s incident-response plan. This includes securing affected systems or devices, preserving evidence for investigation, and evaluating the breach's scope - such as the type of data exposed and the potential risks to patients.
Once the breach is confirmed, HIPAA requires notifying affected individuals promptly - no later than 60 days after discovering the incident. You must also report the breach to the Office for Civil Rights (OCR) and, in some cases, inform the media. Keep detailed records of every action taken, from containment measures to notifications and follow-up efforts.
Treat the incident as an opportunity to strengthen your safeguards. Analyze the root cause, update policies, and revise training materials to prevent similar breaches in the future. Regular assessments and improvements are essential for staying HIPAA-compliant and safeguarding patient privacy.
Author

Lidia Chesnokova, VP of Client Success at PatientPartner, drives patient engagement software strategy and personalized support solutions in healthcare.
Related Articles
Stay Ahead in Patient Engagement
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.
We and selected third parties use cookies or similar technologies for technical purposes and, with your consent, for other purposes as specified in the cookie policy. Use the “Accept” button or close this notice to consent.


